Baylor Takes Preventive Measures After Student Hospitalized With Meningitis
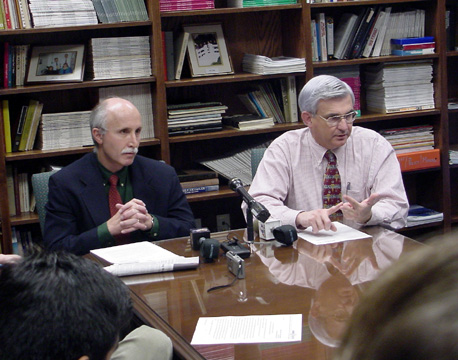
(L to R) Dr. Mark Schwartze, medical director of the Baylor health center, and Dr. Scott Lea, public health officer for the McLennan County Public Health District, met with reporters Wednesday about the university's meningococcal meningitis case.
Baylor University began a series of preventive health measures Nov. 5 after a student was confirmed to have an aggressive form of meningococcal meningitis.
Providence Health Center officials Nov. 7 said the condition of Darrin James Adams, a junior from Pawnee, Okla., has been upgraded from critical to stable.
The university informed all students, faculty and staff of the health concern Nov. 5 and encouraged those who may have had close contact with Adams over the past five to seven days to seek preventive treatment. Dr. Mark Schwartze, health center medical director, secured an ample supply of a single pill (prophylaxis) used in the preventive treatment of the illness. The health center will continue to provide the treatment and alternatives for those who cannot take the single pill during regular hours this week. As of Nov. 7, about 500 students, faculty and staff have taken the post-exposure treatment as a precaution.
The health center also has set up a hotline to answer any questions at (254) 710-4939. Baylor already had its twice-yearly immunization clinic scheduled in two weeks but is working on having the immunizations available sooner, Schwartze said.
Meningitis is an infection of the fluid of a person's spinal cord and the fluid that surrounds the brain. Meningococcal meningitis is a severe form of the disease and can result in brain damage or hearing loss. Common early symptoms of the disease include fever and chills, stiff neck, severe headache, nausea, vomiting, rash and lethargy or mental confusion. If symptoms are present, a person should see a doctor immediately.
The meningococcal bacteria are spread through close personal contacts with a person who is a carrier of the bacteria. Close contacts are household members, as well as those having intimate contact with the affected person through the sharing of drinking glasses, eating utensils or toothbrushes, kissing, coughing and sneezing. In addition, those spending four or more hours with the person for five to seven days before the onset of the disease are considered close contacts.